The skeletal system made of bones and cartilage is a critical component of human anatomy, having its particular functions. Without the bony framework, it might not have been possible to stand or move properly. Our bones grow and develop throughout our lives with the help of osteoclasts and osteoblasts. The regeneration of bones enables your body to mediate bone loss due to bone disease or disorders.
Let’s tell you all the differences between osteoclasts and osteoblasts.
Comparison Table
| Characteristics | Osteoclasts | Osteoblasts |
| Function | Reabsorption | Bone remodeling |
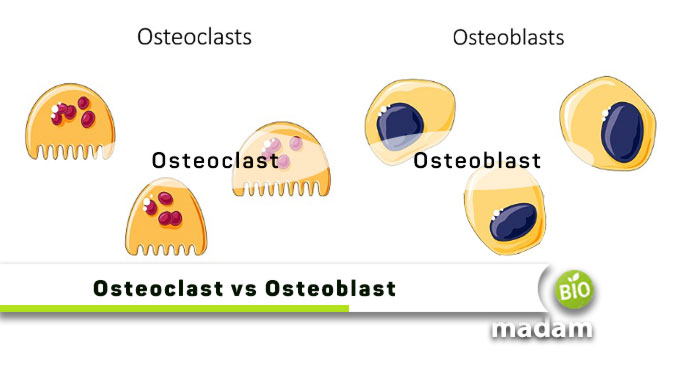
| Nucleus | Multinucleated | Uninucleated |
| Size | Giant | Small |
| Derived From | Hematopoietic cells | Mesenchymal stem cells |
| Osteocyte Formation | No | Yes |
| Osteoid Protein Formation | Yes | No |
What are Osteoclasts?
Osteoclasts are defined as cells that degrade bones to facilitate normal bone regeneration and mediate bone loss by improving their reabsorption. In physiological conditions, osteoclasts break down bone and come from the monocyte/macrophage lineage. They can differentiate into a range of functional cell types and have a high capacity for cell renewal throughout their existence. Osteoclasts are specifically designed to increase absorption in bones. Remodeling of the extracellular matrix plays a significant role in this process. Monocyte fusion produces osteoclasts, which have 2 to 12 nuclei per cell on average. Osteoclast dysfunction causes disorders that resemble osteopetrotic conditions and a lack of bone turnover.

Characteristics and Location
Multiple infoldings of the osteoclast cell membrane create a “ruffled border” in the osteoclast’s vicinity to the bone. Along the ruffled boundary, it secretes acid and proteases that break down the mineral in bone and obliterate the organic matrix. They have 10 to 20 nuclei. By tying their surface integrins to a bone protein known as vitronectin, they form a tight bond with the bone matrix. The osteoclast can create a microenvironment that promotes bone resorption thanks to the close apposition, which closes off a portion of the bone beneath it.
Osteoclasts are located in pits on the surface of the bone termed resorption bays or Howship’s lacunae. A homogenous, “foamy” look to the cytoplasm is a characteristic feature of osteoclasts. The presence of many vesicles and vacuoles accounts for this look. Lysosomes containing acid phosphatase are among the vacuoles in these cells. The osteoclasts are present in Howship’s lacunae, cavities created by the breakdown of the underlying bone.
Process
These cells use chemotaxis to travel to the sites of bone microfracture. The osteoclast’s plasma membrane’s fusion with the underlying bone forms the sealing zone. Belts of specialized adhesion structures known as podosomes surround sealing zones. Integrin receptors, like v3, use the unique amino acid sequence Arg-Gly-Asp in bone matrix proteins, such as osteopontin, to promote attachment to the bone matrix.
The osteoclast releases hydrogen ions through the ruffled border of the resorptive cavity through the activity of carbonic anhydrase enzyme. It helps acidify and speed up the breakdown of the mineralized bone matrix into Ca2+, H3PO4, H2CO3, water, and other substances. Proton pumps, particularly a special vacuolar-ATPase, pump hydrogen ions against a steep concentration gradient.
We can prevent osteoporosis by targeting this enzyme. The matrix’s organic components are also broken down by several hydrolytic enzymes, including those from the cathepsin and matrix metalloproteinase (MMP) groups. Lysosomes allow these enzymes to enter the compartment. Cathepsin K is the most significant of these hydrolytic enzymes.
Examples
- Osteoclasts in bone
- Kupffer cells in the liver
- Histiocytes in lymph nodes
- Langerhans cells in the mucosa
- Hofbauer cells in the skin
- Mucosa in the placenta
- Microglia in the central nervous system
What are Osteoblasts?
Osteoblasts are the cells that produce bones. They are the ones that form the matrix that gives bone its shape out of the three different types of bone cells.
Bone synthesis and mineralization occur during early bone formation, and subsequent bone remodeling by osteoblasts. They are mononucleated cells containing only one nucleus that performs all of its functions. They develop from mesenchymal stem cells.
Through the receptor activator of nuclear factor-B ligand and osteoprotegerin, osteoblasts also play a part in controlling the activity of osteoclasts. Osteoprogenitor cells give rise to osteoblasts.

Characteristics and Location
Numerous elements, including different hormones and locally produced bioactive chemicals following fracture, impact the conversion of osteoprogenitors. These conditions allow osteoprogenitors to proliferate in increases and start differentiating into osteoblasts, which carry out osteogenic tasks. Because osteoblasts are functional cells, they rarely divide and proliferate.
Osteoblasts have a position on top of or close to the existing bone. They create a matrix that develops into a fresh layer of compact and spongy bone tissue that strengthen and thicken the already-existing bone. Osteoblasts eventually become enclosed in the matrix that they themselves make in the case of bones, though. We refer to the cells as osteocytes once this has occurred. A single osteoblast cannot build a bone by itself. Instead, osteoblasts collaborate in communities known as osteons.
Process
Mononucleate cuboidal osteoblasts carry out the role of bone production. Mesenchymal stem cells give rise to osteoblasts, chondrocytes, muscles, fats, tendon and ligament cells. For mesenchymal stem cells to develop into adult osteoblast cells, numerous transcriptional processes must occur. Mesenchymal stem cells commit to the osteoblast phenotype when encountering bone morphogenic proteins (BMPs).
The transforming growth factor – (TGF-) superfamily of proteins, which includes BMPs, acts as morphogens, impacting key processes like neurogenesis, kidney, gut, tooth development, and bone production.
When osteoprogenitor cells begin to differentiate into osteoblasts, they start to express various genetic markers, including the secretion of collagen I, which is necessary for hydroxyapatite to mineralize later creates osteoids, which the osteoblasts then employ to mineralize the bone tissue by causing calcium salts and phosphorus to precipitate from the blood.
Alkaline phosphatase, an enzyme involved in bone mineralization, is also a product of osteoblasts. Increasing its expression correlates with the progression of osteoblast differentiation. Estrogen receptors on osteoblasts allow them to multiply osteoblasts and hence boost fibrous protein formation to provide support and structure.
Examples
- Skull
- Mandible
- Clavicles
Similarities Between Osteoclasts and Osteoblasts
- Osteoblasts and osteoclasts can both be present on bone surfaces.
- They are found in compact and spongy bones.
- The building and dismantling of bones involve osteoblasts and osteoclasts.
Difference Between Osteoclast and Osteoblast
Definition
Osteoclast
An osteoclast is a specific bone cell in charge of resorption.
Osteoblast
Osteoblasts are bone-forming cells that participate in the processes of bone remodeling.
Nucleus
Osteoclast
These cells are multinucleated.
Osteoblast
On the opposite, these cells are mononucleated.
Size
Osteoclast
Osteoclasts are giant cells.
Osteoblast
In contrast, osteoblasts are small in size.
Derived From
Osteoclast
Osteoclasts are the derivation of hematopoietic cells of macrophage lining.
Osteoblast
On the contrary, osteoblasts are the derivation of mesenchymal stem cells.
Function
Osteoclast
Osteoclasts are responsible for bone resorption.
Osteoblast
At the same time, osteoblasts are responsible for bone mineralization and formation.
Osteocyte Formation
Osteoclast
These cells don’t turn into osteocytes.
Osteoblast
After bone production, osteoblasts turn into osteocytes.
Osteoid Protein Formation
Osteoclast
Osteoclasts don’t produce osteoid protein.
Osteoblast
Osteoblasts produce osteoid protein that is generally a fibrous protein to help in the maturation of mineralized bone.
The Bottom Line
Osteoclasts and osteoblasts are important components in the bones to improve absorption and produce new bones. The main difference between osteoclasts and osteoblasts is their contribution to bone health. Osteoclasts increase reabsorption while osteoblasts play a vital role in bone remodeling. Osteoclasts are multinucleated whereas osteoclasts are uninucleated. These cells help keep the bones healthy and save you from bone disorders like osteoporosis, rheumatoid arthritis, and osteoarthritis.

Hello, I would like to introduce myself to you! I am Chelsea Rogers, an experienced blog writer for science articles, holding an MPhil degree. My enthusiasm to grab the best knowledge, let it relate to botany, zoology, or any other science branch. Read my articles & let me wait for your words s in the comment section.